Understanding Diabetes: Types, Insulin, and Healthy Habits
This post is not intended as medical advice. This information is for educational and awareness purposes only. Please consult your doctor or a medical professional for medical advice or if you have or suspect you may have diabetes.
Diabetes is on the rise, and with November being Diabetes Awareness Month, this is the perfect time to bring up the discussion, as 1 in 3 people have prediabetes and may not even realize it.
A common myth about diabetes is that it only happens to people who eat too much sugary food like candy, soda, sweetened coffee, and daily sweet treats. But it’s not that simple.
And while unhealthy eating habits do affect a person’s chances of getting diabetes, this is not the only reason a person can develop diabetes. Diabetes also has a genetic component, and there are several types of diabetes. The most common and well-known types of diabetes are type 1, type 2, and gestational diabetes.
Each type of diabetes shares similarities in that it involves insulin and glucose (blood sugar). Still, each type differs in the way that it comes about and how it affects the individual.
To answer some questions:
What is Diabetes?
Diabetes is a chronic health condition where blood sugar (glucose) levels become too high. The reasons for this vary depending on the type of diabetes. But regardless, in order to control high blood sugar, insulin needs to be present in the bloodstream and able to help glucose enter the cell, so that the cell can absorb the sugar that is in the blood.
If the sugar in the blood does not enter the cells, it will build up in the bloodstream and lead to serious complications. The damage that can result from diabetes can affect the nerves, eyes, hearing, and organs such as the kidneys and heart. It can also lead to frequent infections, ulcers, slow healing, and even death.
What is Insulin?
Insulin is necessary because it is the hormone that moves glucose out of the bloodstream and into the cells for use or storage. The pancreas produces insulin, and if it can't make or maintain sufficient insulin, or if the insulin isn’t functioning effectively, a person’s blood sugar levels will rise, which can lead to serious health complications.
People who have diabetes may also struggle with keeping their insulin balanced. In some cases, too much insulin medication, not eating enough carbs, alcohol use, delayed meals or fasting, and even physical activity can lead to a drop in blood sugar, which can be just as dangerous as blood sugar that is too high.
What is Type 1 Diabetes?
Type 1 diabetes, sometimes called “juvenile diabetes” or “insulin-dependent” diabetes, is an autoimmune disease. Type 1 diabetes is not preventable because a person’s immune system attacks their own insulin-producing beta cells in the pancreas, destroying the cells. This means that a person with type 1 diabetes can't produce enough or sometimes no insulin. Because of this, people who have type 1 diabetes must monitor their blood sugar and take insulin since their bodies are not able to create and maintain their own insulin.
What is Prediabetes?
Prediabetes is the stage before type 2 diabetes is reached as a diagnosis, and it needs to be taken seriously. Many people are prediabetic without realizing it. Prediabetes is when the blood sugar is higher than “normal,” but not high enough to be classified as type 2 diabetes. The good thing is, if caught, prediabetes can be controlled and sometimes even reversed, returning blood sugar levels to the normal range.
What is Type 2 diabetes?
Type 2 diabetes is the most common type of diabetes. It occurs when the body does not use insulin properly, preventing insulin from letting sugar enter the cells. Over time, the pancreas may not produce enough insulin to lower blood sugar levels. This results in glucose (sugar) accumulating in the blood. While genetics play a role, type 2 diabetes can often be prevented or managed through diet and regular exercise. Poor diets high in refined sugar and carbs can lead to insulin resistance, and a lack of exercise also contributes to the condition.
What is Gestational Diabetes?
Gestational diabetes occurs during pregnancy and typically goes away after the baby is born. However, it’s important to get screened and follow your doctor’s advice, because gestational diabetes can cause complications with the pregnancy and delivery.
Medical professionals do not fully understand why some people develop gestational diabetes during pregnancy and others do not. They believe it results from hormone fluctuations during pregnancy due to the placenta, which can impair some people’s bodies from using sugar effectively.
Some medical professionals believe that having extra body weight before pregnancy may play a role, as well as being prediabetic, having PCOS, having gestational diabetes during a previous pregnancy, having a family member who is diabetic, advanced maternal age, or being of Black, Hispanic, Asian, or American Indian descent.
Those who have had gestational diabetes may be at risk for developing type 2 diabetes later in life, so it is important to discuss any health concerns with their provider.
Eating for Diabetes:
Diabetes affects people differently; this is why, if you or someone you know has diabetes, it is critical to work with a medical provider or dietitian who can customize a nutrition plan based on your individual needs. Diabetes is a medically complex disease, and nutrition that works for one person may not work for another.
Your provider or dietitian may recommend eating more lean proteins, low-fat dairy, and non-starchy complex carbohydrates (ex, broccoli, cucumber, tomatoes, etc.). This doesn’t mean giving up the foods you love, but it does mean that you may need to adjust the amount and frequency of how you eat them.
** Note – People may try to sell diabetic meal plans or give them away for free online. I do not recommend buying or following these without your provider’s or dietitian’s approval. As mentioned, diabetes can be very individualized and should be monitored with a medical professional’s guidance.
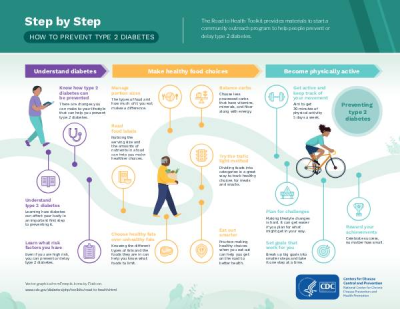
Diabetes Prevention and How to Reduce Diabetes Risk:
Not every type of diabetes can be prevented, but taking steps to improve your overall health can reduce your risk of developing type 2 diabetes, especially if you have already been diagnosed with prediabetes.
Maintaining a healthy body weight can help prevent or manage type 2 diabetes. Physical activity is a great way to stay healthy and maintain a healthy body weight, and it doesn’t need to be demanding. Engaging in any activity that gets you up and moving for at least 30 minutes a day, five days a week, can help keep your body healthy. This can include activities like walking, biking, yoga, tennis, swimming, gardening, or playing with your children outside. Going to the gym or YMCA is another option if you live in an area with seasonal changes or lack access to outdoor spaces. Some communities also have programs for seniors and offer gentle chair exercises.
When it comes to food, eating in a balanced way is very beneficial for your overall health; it’s not just good for preventing diabetes. Eating balanced means that, in general, you focus on getting lean protein, healthy carbs and fats, along with fiber from fruits, vegetables, and whole grains, into your meals and snacks. It is an attempt to focus on limiting less nutritious foods, eating mindful portions, drinking water, and incorporating healthier food options.
Questions to Ask Your Doctor or Dietitian:
If you have recently been diagnosed with diabetes, have a loved one who has been diagnosed, or are curious about how diabetes could affect your health, here is a list of questions that you can ask your provider. You don’t need to ask all of these questions, but some of them may help you understand your chronic illness better.
Do you have a list of vegetables that will be better for my blood sugar?
Which fruits will be best for me to manage my blood sugar?
Do I need to switch to sugar-free foods?
What should I look for on food labels?
How often should I eat?
Do I need to count carbs?
What should my carb portion sizes be?
What would be considered moderation for me, specifically?
Are there any foods I should avoid?
What should my target blood sugar be?
How often should I test my blood sugar?
Do I need insulin?
What should I do if I forgot to take my medication?
What should I do if my blood sugar goes too low?
How can I prevent diabetes related health complications?
What type of exercises should I do and how much?
Should I check my sugar before or after exercise?
Should I eat before or after exercise?
Final Thoughts
This November, take a moment to learn about and share information for Diabetes Awareness Month. Gaining a good understanding of diabetes and its potential impact on your health can help you safeguard your well-being now and in the future. Remember, even small adjustments to your nutrition and daily habits can lead to meaningful improvements.
For More Information, Check Out These Sources:
1 - American Diabetes Association
2 - International Diabetes Federation
3 - World Health Organization Diabetes
4 - CDC National Diabetes Statistics Report
5 - Happy Peach Blog Post (fruit as a carb)
Remember: this post is for informational purposes only and may not be the best fit for you and your personal situation. It shall not be construed as medical advice. The information and education provided here is not intended or implied to supplement or replace professional medical treatment, advice, and/or diagnosis. Always check with your own physician or medical professional before trying or implementing any information read here.